Is Breastfeeding Beneficial to My Baby?
August is National Breastfeeding Awareness Month, dedicated to promoting the benefits of breastfeeding for both mothers and babies. This annual observance raises awareness about its importance provides support to new mothers, and educates communities on how to create environments that encourage and facilitate breastfeeding.
The Significance of National Breastfeeding Awareness Month
It offers numerous health benefits for both infants and mothers. It provides the perfect balance of nutrients tailored to an infant’s needs and plays a crucial role in the emotional bonding between mother and baby. This awareness Month empowers communities to recognize these benefits, correct common myths, and address the challenges mothers often face. The month highlights the need for supportive policies in workplaces, healthcare settings, and communities to ensure that mothers can breastfeed successfully.
Health Benefits of Breastfeeding
It delivers optimal nutrition to babies, providing the right balance of nutrients and immune system support. It strengthens a baby’s defenses, reducing the risk of respiratory infections, ear infections, and gastrointestinal diseases. This can also help lower the risk of chronic conditions like asthma, obesity, type 2 diabetes, and Sudden Infant Death Syndrome (SIDS). It enhances cognitive development, leading to higher IQ scores and better overall brain function.
For mothers, breastfeeding promotes postpartum recovery by helping the uterus contract and return to its pre-pregnancy size, which reduces postpartum bleeding. It also helps mothers burn extra calories, assisting in post-pregnancy weight loss. It reduces the risk of developing breast and ovarian cancers and lowers the likelihood of osteoporosis later in life. Most importantly, it fosters a deep emotional bond between mother and baby, releasing oxytocin and strengthening this connection.
How Pelvic Floor Physiotherapy Supports Breastfeeding
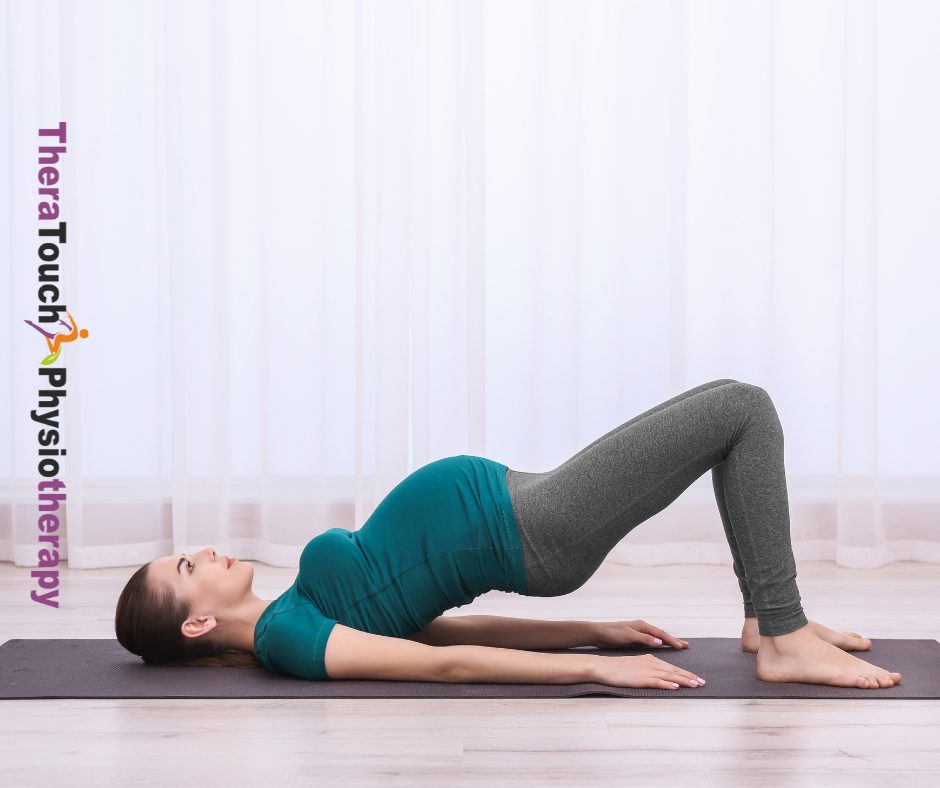
Pelvic Floor Physiotherapy, plays a significant role in supporting mothers during this journey. Pregnancy and childbirth place considerable strain on a woman’s body, especially the pelvic region. These physical changes can lead to discomfort and pain, which can make it more challenging.
By focusing on restoring strength and function to the core & pelvic muscles, pelvic floor physiotherapy helps alleviate pain and improve overall well-being. By addressing issues like poor posture and muscle tension, physiotherapy makes breastfeeding more comfortable and reduces physical stress. Physiotherapists can also employ specific techniques to improve circulation and reduce stress, which can support milk production and make it a more positive experience.
Overcoming Barriers and Challenges
Many mothers encounter significant barriers when breastfeeding. A lack of support from family, healthcare providers, or employers can make it difficult to establish and maintain this practise. Returning to work often presents another challenge, especially when workplaces lack designated breastfeeding areas or flexible schedules.
Cultural attitudes and social stigmas around breastfeeding in public can make mothers feel uncomfortable or embarrassed, discouraging them from continuing. Additionally, physical challenges like sore nipples, low milk supply, or mastitis can make it painful and difficult.
Fed is best. A well-nourished baby is the priority, no matter how they are fed.
Providing Support and Resources for Breastfeeding Mothers
To help mothers overcome these challenges, communities must provide comprehensive support. During this month, organizations and communities come together to offer resources, guidance, and encouragement. Healthcare professionals, including lactation consultants and physiotherapists, play a crucial role in supporting mothers, offering personalized advice and helping to manage any physical discomfort associated with it.
Employers can support breastfeeding mothers by offering flexible work schedules, providing designated lactation rooms, and implementing adequate maternity leave policies. Public awareness campaigns during this Awareness Month also play a key role in normalizing it and promoting supportive environments for breastfeeding mothers.
National Breastfeeding Awareness Month celebrates the many benefits of breastfeeding while recognizing the challenges that many mothers face. By educating communities about the importance of breastfeeding, and providing essential resources, we can ensure that every mother feels empowered to provide the best possible start for her baby. During this month, we come together to create a world where breastfeeding is supported, celebrated, and accessible to all mothers.