Polycystic Ovary Syndrome (PCOS) Awareness Month
September is PCOS Awareness Month, a time when we focus on understanding and supporting women who live with Polycystic Ovary Syndrome (PCOS). This month brings us together to raise awareness about PCOS, share knowledge, and offer comfort to those who navigate its challenges every day. By shining a light on PCOS, we can help women find the support they need to manage their symptoms and live full, healthy lives.
Understanding PCOS
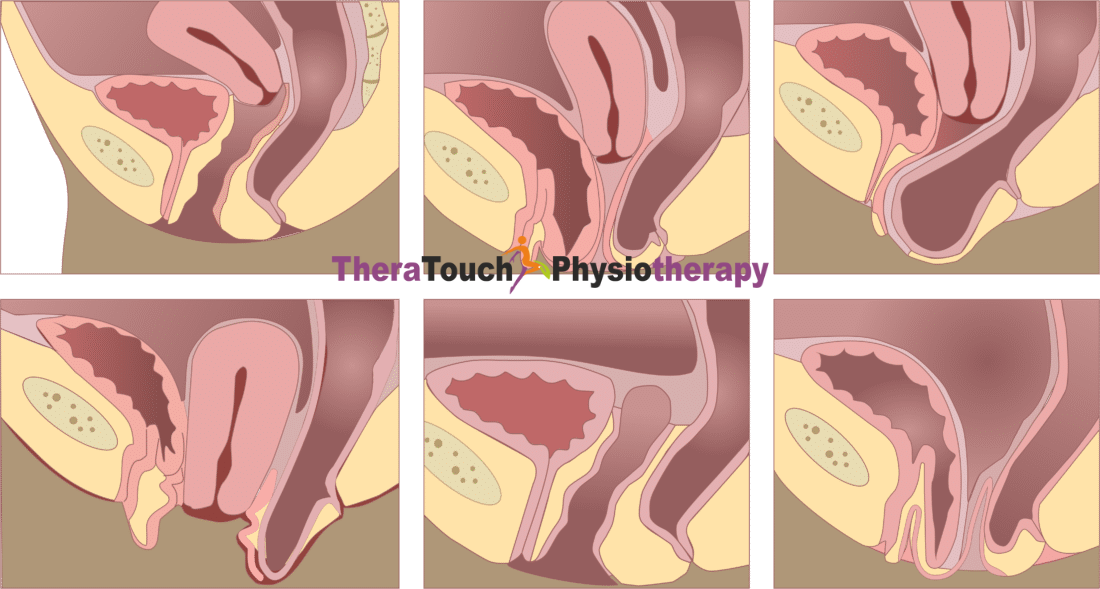
PCOS is a condition that touches the lives of many women, though it’s often misunderstood. When you have PCOS, your body experiences a hormonal imbalance that can lead to various symptoms, from irregular periods and fertility issues to weight gain and skin changes. These symptoms can vary widely, making each woman’s experience with PCOS unique. Yet, despite how common it is, PCOS often goes undiagnosed, leaving many women feeling confused and isolated as they try to understand what’s happening to their bodies.
Early diagnosis makes a world of difference in managing PCOS. When you know what you’re dealing with, you can start taking steps to manage your symptoms and protect your long-term health. Doctors often diagnose PCOS by looking at your symptoms, checking hormone levels through blood tests, and sometimes using ultrasound to look at your ovaries. While there isn’t a cure for PCOS, there are many ways to manage it, allowing you to live well despite the challenges.
How Physiotherapy Can Help
Physiotherapy offers a gentle yet powerful way to manage the symptoms of PCOS. Many women with PCOS face challenges like weight gain, insulin resistance, and even chronic pain, particularly in the pelvic area. By working with a physiotherapist, you can address these issues head-on, improving your physical health and overall well-being.
When you have PCOS, staying active is incredibly important. Regular exercise helps manage your weight and improves how your body handles insulin, both of which are key to managing PCOS. A physiotherapist can help you develop a personalized exercise plan that fits your needs and respects the unique challenges you might face, like joint pain or fatigue. By focusing on exercises that build strength, improve flexibility, and boost cardiovascular health, you can take control of your symptoms in a way that feels empowering and achievable.
For those of you who experience pelvic pain, pelvic floor physiotherapy can offer significant relief. This specialized therapy focuses on strengthening and relaxing the muscles in your pelvic area, helping to reduce pain and improve your daily comfort. Whether you’re dealing with pain during your period, discomfort during exercise, or pain in your daily life, pelvic floor physiotherapy can help you find relief and feel more in tune with your body.
Beyond the physical benefits, physiotherapy also supports your emotional well-being. Dealing with a chronic condition like PCOS can feel overwhelming, but regular sessions with a physiotherapist provide a safe and supportive space to focus on your health. This dedicated time helps you feel more in control, which can lift your spirits and reduce the stress that often comes with managing a chronic condition.
Overcoming the Challenges of PCOS
Living with PCOS isn’t easy, and it’s okay to acknowledge that. The symptoms can be tough to manage, and the emotional toll can be heavy. But you don’t have to face it alone. PCOS Awareness Month reminds us all that there is a community of support out there, ready to offer understanding, advice, and encouragement.
If you’re feeling overwhelmed by your symptoms, reaching out for support can make all the difference. Whether it’s talking to your healthcare provider, joining a support group, or connecting with others who understand what you’re going through, these connections can help you feel less isolated and more empowered to manage your condition.
The Power of Awareness and Advocacy
By raising awareness about PCOS, we can create a world where women with PCOS feel seen, supported, and understood. Advocacy during this month isn’t just about education; it’s about creating real change—pushing for more research, better healthcare services, and policies that support women’s health.
When we talk openly about PCOS, we help to break down the stigma and misinformation that so often surrounds it. We make it easier for women to seek help, to ask questions, and to take control of their health. And we remind everyone that managing PCOS is not just about surviving, it’s about thriving.
PCOS Awareness Month is our chance to come together and show women with PCOS that they are not alone. With the right support and knowledge, you can manage your symptoms, reduce your health risks, and live a full, vibrant life. Physiotherapy is just one of the many tools available to help you on this journey, offering comfort, relief, and a path to better health. This month, let’s celebrate the strength and resilience of every woman living with PCOS and commit to building a world where every woman can access the care and support she deserves.