When It Feels Like a UTI but Isn’t
You feel a constant urge to pee. Sometimes it burns when you go, and sometimes the discomfort is just there, lingering like a dull ache in your lower abdomen. Naturally, your first thought is a urinary tract infection. You head to the doctor, get a urine test, and wait for the results. But they come back clean. No infection. No bacteria. Yet the pain hasn’t left. If this keeps happening to you, you’re not imagining it. That discomfort that feels exactly like a UTI but doesn’t respond to antibiotics may be coming from your pelvic floor muscles not your bladder.
The Real Source of the Discomfort
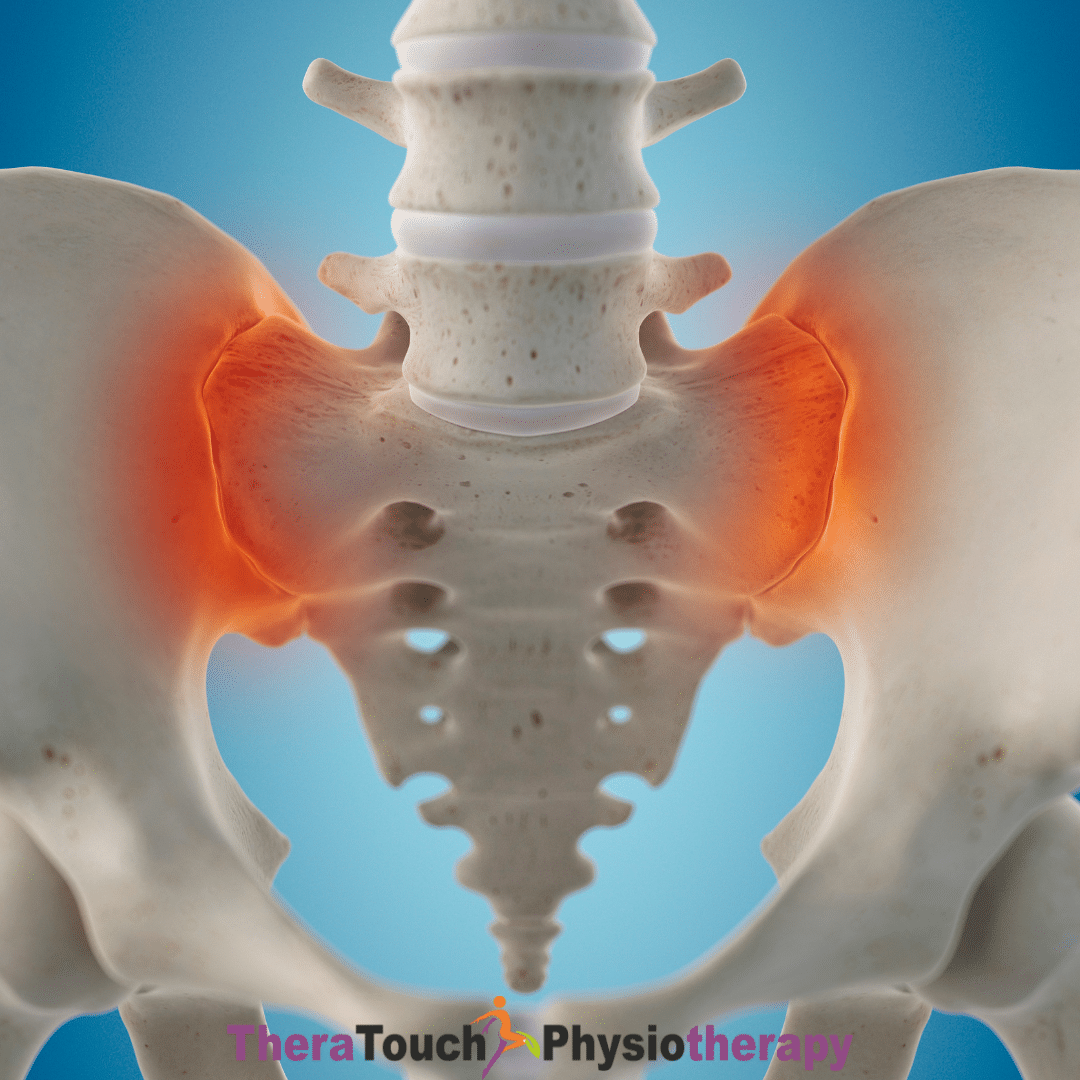
Your pelvic floor is a group of muscles located at the base of your pelvis. These muscles help support your bladder, bowel, and reproductive organs. They also play a major role in how your bladder functions. When your pelvic floor becomes too tight, overworked, or dysfunctional, it can irritate the nerves surrounding the bladder and urethra. This nerve irritation sends mixed signals to your brain, making your body feel like something is wrong with your urinary system even when there is no infection. You may feel like you constantly need to urinate, even right after you just did. You may feel burning or stinging during urination, pressure deep in the pelvis, or general discomfort that feels eerily like a UTI. But because there’s no bacterial infection to treat, antibiotics won’t help.
Why Antibiotics Aren’t Solving the Problem
If your tests consistently show no bacteria, but you keep experiencing the same pain, it’s a strong sign that the issue isn’t coming from an infection. Your pelvic floor muscles might be holding too much tension or reacting to stress, past trauma, posture changes, or even past infections that left behind lingering hypersensitivity. In this case, no medication can ease the muscle tightness or correct the miscommunication between your nerves and bladder. That’s why antibiotics often fail to bring relief. They are targeting a problem that doesn’t exist while the real source of your pain remains untreated.
The Role of Pelvic Floor Physiotherapy
Pelvic floor physiotherapy gives you a clear, non-invasive path toward healing. During your sessions, your physiotherapist will assess how your pelvic muscles are functioning and how they may be contributing to your symptoms. You’ll learn how to release unnecessary tension, how to coordinate your muscles properly, and how to calm your nervous system’s hypersensitive response to normal bladder activity. Treatment may include breathwork, gentle internal or external manual therapy, posture retraining, movement strategies, and exercises to improve pelvic blood flow and reduce nerve irritation. Over time, this helps reduce that false sense of urgency, relieves the burning sensations, and gives you back a sense of control and comfort.
Breaking the Cycle and Finding Relief
Living with ongoing UTI-like symptoms that don’t respond to medication can feel frustrating and confusing. You may start to doubt your own body or feel anxious every time you sense a twinge in your bladder. But you are not alone, and your pain is valid. Pelvic floor dysfunction is a common but often overlooked cause of this type of discomfort. The good news is that with the right guidance, it is also highly treatable. Physiotherapy doesn’t just mask the symptoms. It addresses the root cause, gently retrains your body, and helps you return to your normal routines without fear or discomfort. If you’re tired of cycling through antibiotics or being told that everything is “normal” when you still feel pain, pelvic floor physiotherapy may be the key to long-term relief.