How can I get Relief from Constipation?
Constipation can be a frustrating and uncomfortable condition that affects many people. It involves infrequent or difficult bowel movements and often leaves you feeling bloated and sluggish. While occasional constipation is normal, persistent issues can disrupt your daily life. Although factors like diet, hydration, and physical activity play significant roles, an often-overlooked factor is the health of your pelvic floor muscles.
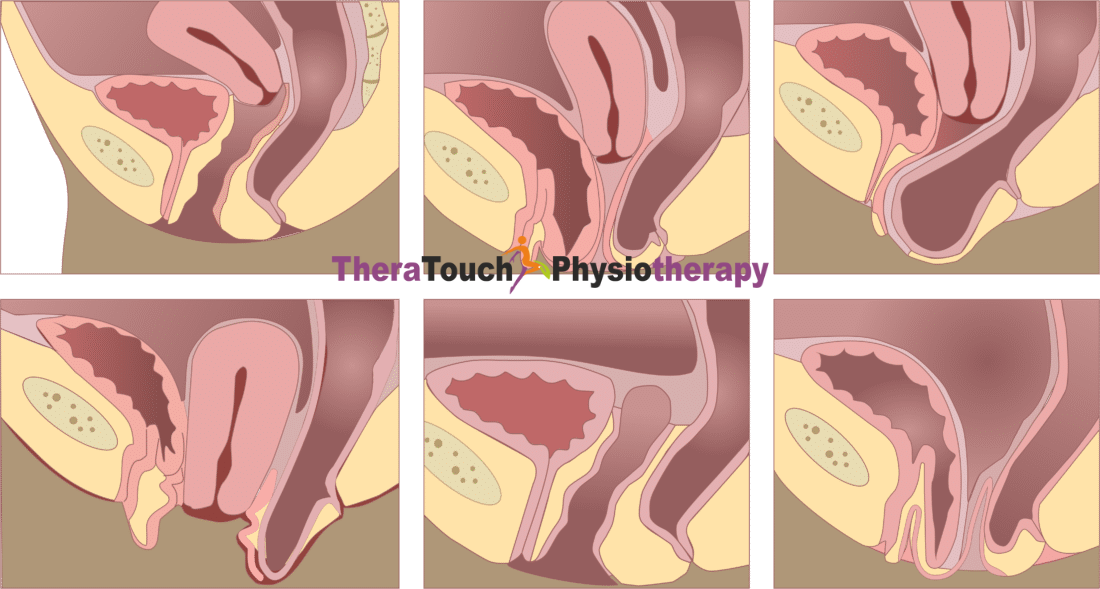
How the Pelvic Floor Affects Digestion
Your pelvic floor muscles form a supportive hammock at the base of your pelvis, holding up the bladder, rectum, and for women, the uterus. These muscles are essential for controlling the release of urine and stool. When these muscles function correctly, they relax to allow stool to pass through the rectum and out of your body. However, if these muscles are too tight, weak or dysfunctional, they can contribute to constipation by interfering with this process.
The Benefits of Pelvic Floor Physiotherapy
Pelvic floor physiotherapy targets the underlying issues causing constipation by focusing on the pelvic floor muscles. A trained physiotherapist assesses these muscles and creates a personalized treatment plan to address any dysfunction they find in you and restore normal function.
Relaxing Tight Muscles
Pelvic floor physiotherapy often involves manual therapy, where the therapist applies gentle pressure and manipulation to the pelvic floor muscles and surrounding tissues. If your muscles are too tight, this therapy can help them relax and release tension. This relaxation makes bowel movements easier and more comfortable.
Strengthening Weak Muscles
For those with weak pelvic floor muscles, the therapist introduces exercises designed to strengthen these muscles. Strengthening the pelvic floor provides better support for the pelvic organs and enhances bowel function. These exercises, often including Kegel exercises, help improve muscle control and coordination, making it easier to pass stool without straining.
Using Biofeedback for Better Control
Biofeedback is another effective tool in pelvic floor physiotherapy. It involves using sensors to give you real-time feedback on your muscle activity. This feedback helps you learn how to properly engage and relax your pelvic floor muscles during bowel movements. Additionally, your physiotherapist will teach you optimal breathing and posture techniques, which are crucial for facilitating easier bowel movements.
Practical Tips for Managing Constipation
In addition to pelvic floor physiotherapy, you can make several lifestyle changes to manage and prevent constipation. Staying hydrated by drinking plenty of water helps soften stool, making it easier to pass. Eating a fiber-rich diet, including fruits, vegetables, and whole grains, promotes regular bowel movements. Fiber adds bulk to the stool and supports a healthy digestive system.
Regular exercise also plays a key role. Physical activity stimulates your intestines, helping move stool through the colon more efficiently. Even simple activities like walking can make a big difference. Establishing a routine, such as going to the bathroom at the same time each day—ideally after meals—can also help. This routine leverages your body’s natural digestive rhythms to encourage regular bowel movements.
“I Love You” (ILU) Abdominal Massage
Perform the “I Love You” (ILU) Abdominal Massage for constipation, loose bowels, and generalized pelvic and abdominal pain. Always massage from right to left, using soap in the shower or cream on your fingertips.
Begin by forming the letter “I.” Stroke with moderate pressure from your left ribcage down to your left hipbone, repeating this motion 10 times.
Next, form the letter “L.” Stroke with moderate pressure from your right ribcage, moving underneath the ribcage to the left, and down to your left hipbone. Perform this motion 10 times.
Finally, form the letter “U.” Stroke 10 times from your right hipbone up to your right ribcage, across to your left ribcage, and down to your left hipbone.
Finish the massage by gently massaging around your belly button in a clockwise circular motion for 1-2 minutes to stimulate your small intestine. Do this massage once daily for best results.
When to Seek Professional Help
If you struggle with chronic constipation or experience severe symptoms such as pain during bowel movements, blood in your stool, or unexplained weight loss, seek professional help. A pelvic floor physiotherapist can provide specialized care tailored to your needs, helping you find relief from persistent symptoms.
Constipation is a common issue, but it’s manageable with the right approach. Pelvic floor physiotherapy offers a powerful way to address constipation by focusing on the muscles that play a critical role in bowel movements. With techniques like manual therapy, strengthening exercises, biofeedback, and education, you can improve muscle function and achieve lasting relief. Combine this with healthy habits such as staying hydrated, eating a fiber-rich diet, and staying active, and you can enhance your digestive health and overall well-being. If you’re dealing with constipation, consider seeking help from a healthcare professional and explore the benefits of pelvic floor physiotherapy for a more comfortable life.