Pelvic Organ Prolapse Awareness Month
June is Pelvic Organ Prolapse (POP) Awareness Month, a crucial time dedicated to educating women about this often-misunderstood condition. Pelvic organ prolapse occurs when the muscles and tissues supporting your pelvic organs weaken, causing one or more of these organs to drop or press into or out of your vagina.
What is Pelvic Organ Prolapse?
Pelvic organ prolapse is a condition where your pelvic organs (bladder, uterus, rectum, and bowel) slip out of their normal position due to weakened supporting structures including pelvic floor muscles. This can lead to discomfort, urinary issues, and other complications. It is more common in women who have given birth, especially those who have had multiple vaginal deliveries.
Who is susceptible to pelvic organ prolapse?
Pelvic organ prolapse (POP) can occur in individuals of any gender, though it is more prevalent in women and people assigned female at birth (AFAB). Men and those assigned male at birth (AMAB) may also experience conditions like bladder and rectal prolapse.
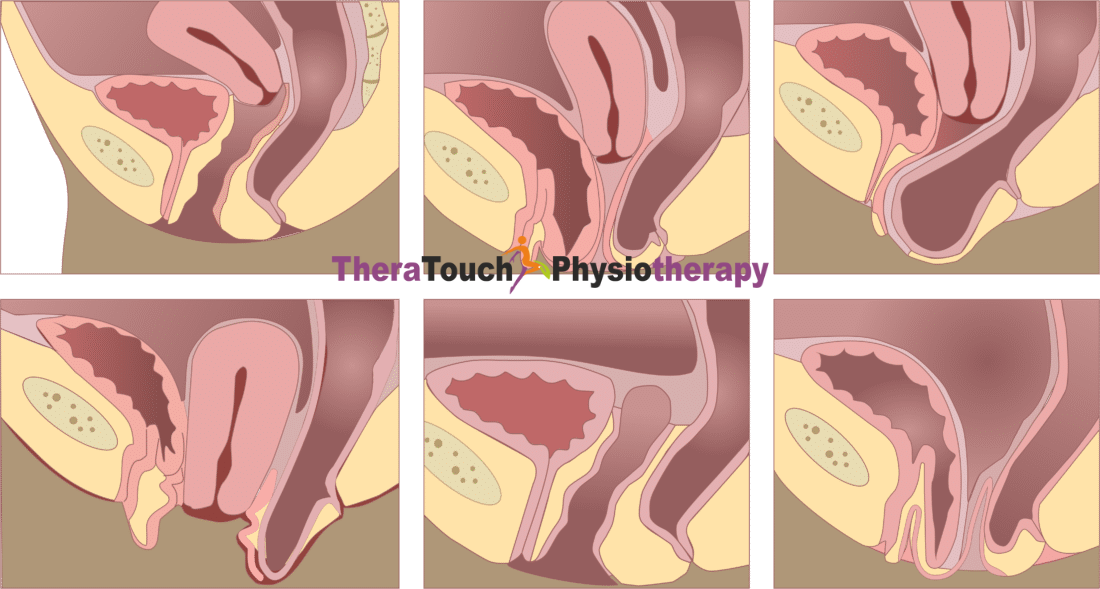
What are the types of pelvic organ prolapse that exist?
Generally, the type of prolapse you experience depends on the location of the weaknesses in your supporting structures including the pelvic floor and the organs that are affected. The severity and symptoms can vary based on these factors. These are the types;
- Anterior vaginal wall prolapse (cystocele): When the supporting structures including the pelvic floor muscles above the vagina weaken, the bladder can shift out of position and press against the vaginal wall. This condition, known as cystocele, is the most common form of pelvic organ prolapse (POP).
- Uterine prolapse: Weakened supporting structures including the pelvic floor can cause the uterus to descend into the vaginal canal.
- Posterior vaginal wall prolapse (rectocele): Weakness in the supporting structures including the pelvic floor muscles between the vagina and rectum can cause the rectum to protrude into the back wall of the vagina. This condition is referred to as rectocele.
- Enterocele: A weakening of the supporting structures including the pelvic muscles can result in the small intestine bulging into the upper part or back wall of the vagina.
- Urethrocele: Weakened supporting structures including the pelvic floor muscles can cause the urethra, the tube that carries urine from the bladder to outside the body, to sag. This condition often occurs alongside a cystocele.
- Vaginal vault prolapse: Sometimes, the top part of the vagina (vaginal vault) can drop into the vaginal canal due to the weakening of the supporting structures including the pelvic floor muscles.
Common symptoms include:
Pelvic organ prolapse (POP) can manifest with a variety of symptoms, often depending on the specific organs involved and the severity of the prolapse. Some of them are;
- A bulge or protrusion in your vaginal area
- A feeling of pressure or fullness in your pelvic area
- Urinary incontinence or retention
- Difficulty with bowel movements
- Abdominal /Pelvic / Back pain
- Discomfort or pain during intercourse
Causes and Risk Factors
The primary cause of POP is the weakening of your supporting soft tissue & pelvic floor muscles, which can occur due to:
- Childbirth: Especially with multiple or complicated deliveries.
- Aging: Muscle tone naturally decreases with age.
- Menopause: Lower estrogen levels can weaken your pelvic tissues.
- Hysterectomy: Removal of the uterus can sometimes increase risk of prolapse of your other organs.
- Chronic Coughing or Constipation: These conditions increase pressure on your pelvic floor.
Treatment Options
Non-Surgical Treatments
For individuals experiencing pelvic organ prolapse (POP), there are several non-surgical treatment options available. These approaches aim to alleviate symptoms, improve pelvic floor function, and enhance quality of life without the need for invasive procedures. These are;
Pelvic Floor Physiotherapy: Strengthening your pelvic floor muscles can alleviate mild to moderate symptoms.
Pessary Devices: A pessary is a device inserted into your vagina to support the prolapsed organs.
Lifestyle Changes: Maintaining a healthy weight, limiting heavy lifting, and managing constipation can help reduce symptoms.
Surgical Treatments
When non-surgical treatments are insufficient to manage pelvic organ prolapse (POP) or the condition is more severe, surgical intervention may be necessary. Your options are;
Pelvic Floor Repair Surgery: These are procedures to repair weakened/lax supporting soft tissues.
Hysterectomy: In severe cases of uterine prolapse, removing the uterus may be recommended by specialists.
Minimally Invasive Surgeries: Laparoscopic or robotic surgeries to correct prolapse with shorter recovery times.
How Pelvic Floor Physiotherapy Helps
Pelvic floor physiotherapy can be a highly effective treatment for pelvic organ prolapse, especially in mild to moderate cases. This specialized form of physical therapy focuses on strengthening your pelvic floor , core & pelvic muscles, improving their function, and reducing the symptoms of POP.
Benefits of Pelvic Floor Physiotherapy
Pelvic floor physiotherapy provides numerous detailed benefits for improving pelvic health. By engaging in targeted exercises, you strengthen your pelvic floor muscles, which are crucial for supporting your pelvic organs effectively. This increased muscle strength not only improves support but also enhances muscle coordination, making everyday activities easier and more comfortable. Many women find that consistent physiotherapy sessions lead to a significant reduction in symptoms such as urinary incontinence, pelvic pressure, and pain. What’s more, this non-invasive treatment option avoids the risks and recovery time associated with surgery, offering a safe and effective path to better pelvic health and overall quality of life.
Prevention of Pelvic Organ Prolapse
Preventing pelvic organ prolapse (POP) involves several proactive measures that can effectively reduce the risk of developing this condition. Regular pelvic floor exercises, such as Kegels, are crucial as they strengthen your pelvic muscles, providing better support for your pelvic organs.
Maintaining a healthy diet rich in fiber and staying hydrated help prevent constipation, which can strain your pelvic floor muscles. Weight management is also important to avoid unnecessary pressure on your pelvic floor. Using proper lifting techniques and minimizing heavy lifting whenever possible can further protect against pelvic floor strain.
Finally, quitting smoking is essential as it can prevent chronic coughing, which puts additional stress on your pelvic floor muscles. By adopting these preventive strategies, you can significantly enhance your pelvic health and reduce the likelihood of developing pelvic organ prolapse.
TheraTouch offers specialized pelvic floor physiotherapy among others to help manage and treat Pelvic Organ Prolapse (POP). We provide personalized care and support to improve your pelvic health and quality of life. Remember, early intervention can make a significant difference. If you suspect you may have POP, don’t hesitate to seek medical advice. We are here to help.