How Do I Use Kegel Weights?
Last week we talked about what Kegels were and how to do them. This week let’s talk about how to use Kegel Weights. Kegel weights can be a fantastic addition to your routine. Let me walk you through everything you need to know about using Kegel weights effectively.
What Are Kegel Weights?
Kegel weights, also known as pelvic floor weights or vaginal weights, are small, weighted devices designed to help you strengthen your pelvic floor muscles. They come in various shapes and sizes, and you can gradually increase the weight as your muscles get stronger. Using these weights can lead to improved bladder control, enhanced sexual pleasure, and better overall pelvic health.
Choosing the Right Kegel Weight for You
When you’re just starting out, it’s important to choose a weight that’s appropriate for your current strength level. Most Kegel weight sets come with a range of weights, typically starting from around 25 grams and going up to 100 grams or more. If you’re new to Kegel exercises, starting with a lighter weight is a good idea. As you progress, you can gradually move to heavier weights to continue challenging your muscles.
Preparing for Your Kegel Weight Session
Before you start using your Kegel weights, it’s essential to prepare both your body and the weights themselves. Begin by emptying your bladder to avoid any discomfort during your exercises. Next, make sure to wash your hands thoroughly with soap and water. It’s also a good idea to clean the Kegel weight with mild soap and water to maintain hygiene.
How to Insert the Kegel Weight
Finding a comfortable position is key for a successful Kegel weight session. You might prefer lying down with your knees bent, standing with one leg raised, or squatting. Whichever position you choose, applying a water-based lubricant to the weight can make insertion smoother. Gently insert the weight into your vagina, aiming for about two inches deep. If your Kegel weight has a retrieval string, make sure it’s accessible for easy removal.
Performing Kegel Exercises with Your Weight
Once the weight is in place, it’s time to start your Kegel exercises. Begin by squeezing your pelvic floor muscles as if you’re trying to lift the weight upwards. Hold the contraction for about 5 seconds, then relax for the same amount of time. Repeat this process 10-15 times. As you build strength, you can gradually increase the duration of the hold to 10 seconds, with 10-second rest periods in between.
Removing the Kegel Weight
When you’re finished with your exercises, it’s time to remove the Kegel weight. Make sure you’re in a relaxed state and take deep, calming breaths. Gently pull the weight out using the retrieval string, or if there’s no string, carefully use your fingers to remove it. After removal, clean the weight with mild soap and water, and store it in a clean, dry place.
Tips for Getting the Most Out of Your Kegel Weight Routine
Consistency is crucial when it comes to strengthening your pelvic floor muscles. Aim to use your Kegel weights at least three times a week for the best results. If you experience any discomfort or pain, it’s important to stop and consult with a healthcare professional. Progress gradually by increasing the weight only when you feel ready, and always listen to your body.
Common Questions About Kegel Weights
Question: How long should you use them each day?
Ans: Starting with 10-15 minutes per session is a good guideline. Over time, you can extend this duration as your muscles become stronger.
Question: Is Kegel weights safe to use during pregnancy?
Ans: It’s always best to consult with your healthcare provider before starting any new exercise regimen during pregnancy.
Question: How do I know if I’m using the right weight?
Ans: The right weight will offer gentle resistance without causing discomfort. If the weight falls out easily, you might need a lighter option. Also, if the weight feels too easy, it might be time to move up to a heavier weight.
Using Kegel weights can be a highly effective way to strengthen your pelvic floor muscles and improve your overall health. By following these steps and incorporating Kegel weights into your routine, you’re taking an important step toward better pelvic health. Remember, consistency and proper technique are essential for achieving the best results.
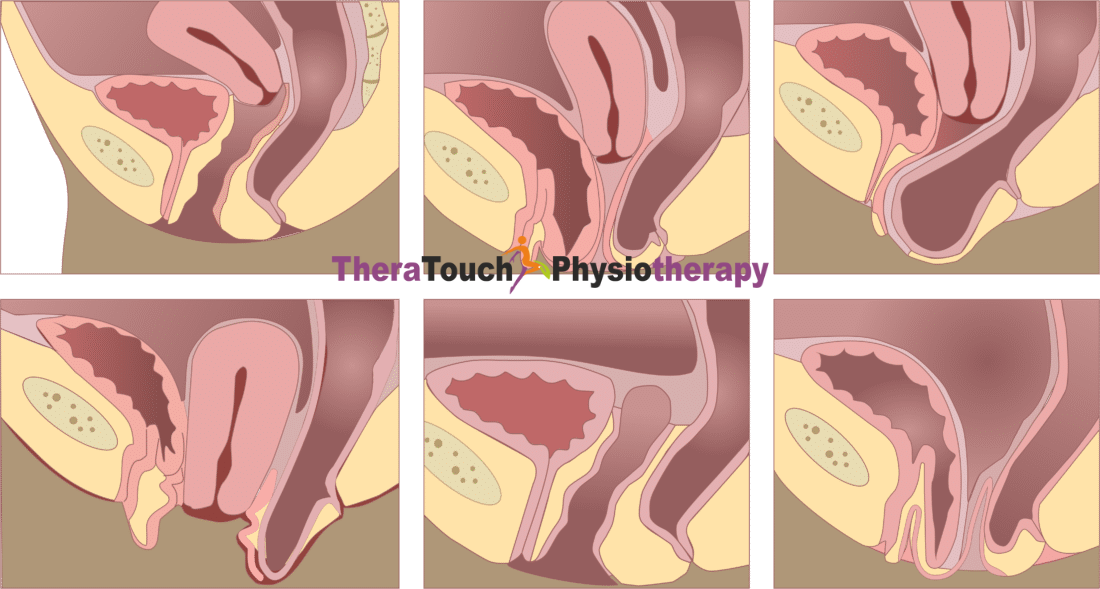
Also, consider seeing a Pelvic Floor Physiotherapist to ensure you are doing kegels correctly and more importantly, relaxing fully after your kegels. Doing kegels incorrectly and not relaxing well can lead to some pelvic floor dysfunction so seek professional help if you need it. Be proactive not reactive!!!
Feel free to leave a comment or ask any questions you might have for this week’s blog. I’m excited to hear about your experiences with Kegel weights!