How To Fix Bad Posture
In today’s digital age, it’s all too common to find ourselves slouching over screens. Whether at a desk, on the couch, or even in bed. Poor posture has become the norm for many, but that doesn’t mean it’s something you should accept as part of your daily life. Unlike a fleeting problem that might resolve itself, your posture won’t fix itself without deliberate effort. To avoid the range of issues associated with poor posture, such as chronic back pain, headaches, and even digestive problems, you need to be proactive.
Consequences of Poor Posture
Your posture affects much more than how you looks. It plays a crucial role in your overall health. When you slouch or hunch over, it places undue strain on your spine and surrounding muscles. This misalignment can lead to chronic back pain, leaving you feeling uncomfortable and restricted. Poor posture also contributes to frequent headaches due to tension in your neck and shoulders. A hunched posture compresses your abdominal organs, potentially causing digestive issues and discomfort. Moreover, poor posture can make you feel more tired and stressed, impacting your mood and productivity.
Physiotherapy Can Transform Your Posture
Physiotherapy is a powerful tool in correcting poor posture and alleviating related problems. Here’s how it can make a difference:
Personalized Assessment and Targeted Treatment
A physiotherapist starts by conducting a thorough assessment to identify specific issues or imbalances in your posture. This personalized evaluation allows them to create a targeted treatment plan that addresses your unique needs. They’ll educate you on proper posture techniques and how to incorporate these into your daily routine.
Customized Exercise Programs
Your physiotherapist will design an exercise program tailored to strengthen the muscles that support good posture, such as your core, back, and shoulders. They’ll also include stretches to relieve muscle tension and improve flexibility, helping you maintain better alignment.
Manual Therapy for Immediate Relief
Techniques like massage and joint mobilization can provide immediate relief by reducing muscle tension and improving mobility. This hands-on approach makes it easier for you to maintain good posture and reduces discomfort.
Ergonomic Advice
If you work at a desk or from home, your physiotherapist can offer practical ergonomic advice to optimize your workspace. This might include adjusting your chair, desk, and computer setup to support better posture and reduce strain.
Ongoing Support and Progress Monitoring
Regular follow-up appointments allow your physiotherapist to monitor your progress, adjust your treatment plan as needed, and offer ongoing support and motivation to keep you on track.
Practical Tips for Improving Your Posture on Your Own
While physiotherapy is highly effective, you can also take several steps on your own to enhance your posture. Incorporate these habits into your daily routine to make a significant difference:
Be Mindful of Your Posture
You have to regularly check in with yourself throughout the day. When sitting, keep your back straight, shoulders back, and feet flat on the floor. When standing, distribute your weight evenly on both feet and avoid locking your knees.
Take Frequent Breaks
If you’re working at a desk or using screens often, make it a habit to stand up, stretch, and move around every 30 minutes. Set a timer if necessary to remind yourself to take breaks and avoid prolonged sitting.
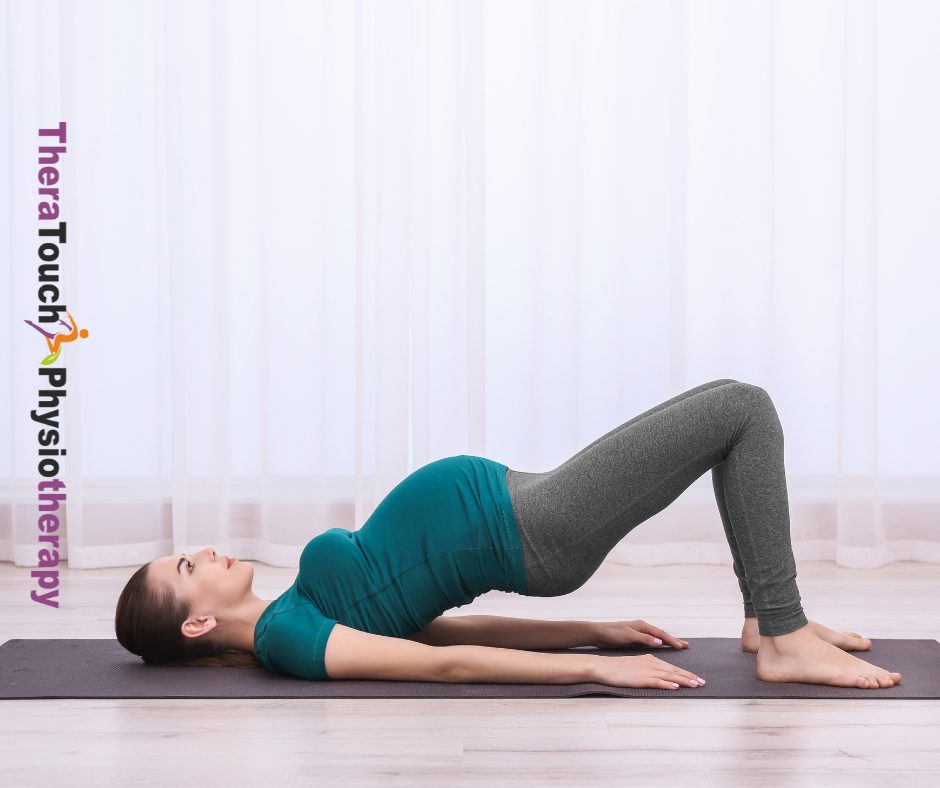
Strengthen Your Core
You have to engage in core-strengthening exercises, such as planks and bridges, to provide better support for your spine. A strong core helps maintain proper alignment and reduces strain on your back.
Incorporate Regular Stretching
Make sure to add stretching exercises to your routine to relieve muscle tension. Focus on areas that are commonly tight due to poor posture, like the chest, shoulders, and lower back. Stretching helps improve flexibility and reduces discomfort.
Use Ergonomic Furniture
Invest in a chair that supports your lower back and an adjustable desk if possible. Ensure that your computer screen is at eye level to reduce neck strain and promote better it.
Practice Good Habits
Pay attention to how you sit, stand, and move throughout the day. Use proper body mechanics when lifting objects—keep your back straight and bend at the knees. Also, ensure your mattress and pillows support a neutral spine position while you sleep.
Your posture is a vital aspect of your overall health, and it won’t improve on its own. By taking proactive steps and seeking professional help from a physiotherapist, you can correct poor posture and prevent related health issues. Start integrating good habits into your daily routine and consider scheduling a session with a physiotherapist here at TheraTouch for personalized guidance will be a good step. With consistent effort and the right support, you can achieve better and enjoy a healthier, more comfortable life.