Physiotherapy for Sacroiliac (SI) Joint Dysfunction: Finding Relief
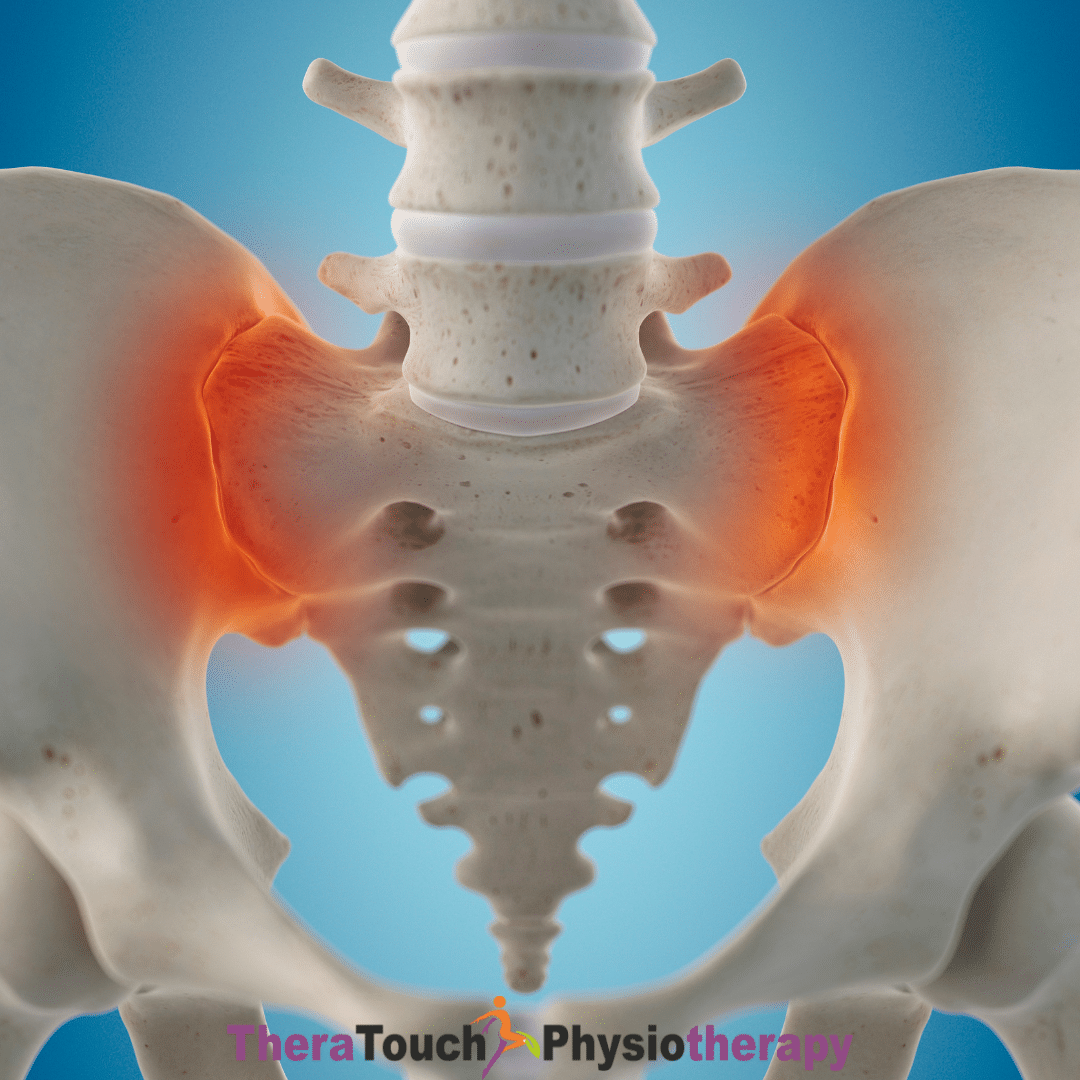
Your sacroiliac (SI) joints may be small, but they play a powerful role in your ability to move comfortably through life. These joints sit where your spine connects to your pelvis, one on each side and they serve as essential shock absorbers every time you walk, twist, bend, or shift your weight. Although they only allow a small amount of motion, their ability to transfer forces between your upper body and your legs makes them critical to daily movement.
When your SI joints move too much or too little, they can throw your entire pelvic system out of balance. This imbalance can lead to deep, nagging pain in your lower back, hips, buttocks, or even your groin. If you’ve ever been told you have sciatica but your pain doesn’t travel far down the leg, your SI joint may actually be the root cause.
Why Sacroiliac Joint Dysfunction Happens
Sacroiliac joint dysfunction doesn’t appear suddenly, it builds over time. If you’ve been pregnant, experienced a fall or accident, had changes in joint flexibility, or carried heavy loads with poor form, your SI joint may have been affected. Even something as subtle as wearing shoes with uneven soles can shift how weight moves through your pelvis. When one SI joint carries more load than the other, the muscles surrounding it start to react. They tighten to protect the area, and that tension begins a cycle. As your muscles stiffen, they pull your pelvis out of alignment. That misalignment creates even more muscle tension and eventually, chronic discomfort or pain.
How Physiotherapists Identify Sacroiliac Joint Dysfunction
Your body tells a story in how it moves and your physiotherapist knows how to listen. Rather than just looking at where you feel pain, your therapist observes how you move through common actions like walking, climbing stairs, or rising from a chair. They pay attention to how your hips shift, how your spine rotates, and whether one side of your body moves differently than the other. By palpating your pelvis and spine, testing muscle strength, and assessing joint mobility, your physiotherapist identifies subtle imbalances. They also rule out other conditions like a herniated disc or hip joint problems to make sure they’re targeting the true source of your discomfort.
Hands-On Therapy to Restore Balance
To help your Sacroiliac joint move better, your physiotherapist begins with hands-on care. These manual therapy techniques restore healthy motion between your sacrum and ilium. They might use methods like muscle energy techniques, where you gently contract a muscle while the therapist uses resistance to realign your joint. Or they may apply light pressure through a strain-counter strain or directional release technique to ease tension without triggering pain. This kind of gentle mobilization is key. Your body doesn’t need force, it needs precision and subtle correction. By restoring mobility to the joint and calming the surrounding muscles, you give your pelvis a fresh start.
Rebuilding Strength and Stability
Once your Sacroiliac joint starts to move freely again, it’s time to teach your body how to keep it that way. That’s where targeted strengthening comes in. Your core muscles including the transverse abdominis, multifidus, pelvic floor, and diaphragm must coordinate with your glutes to create a strong, stable base for every movement you make. You’ll work with your physiotherapist on exercises that feel simple but are deeply effective. Things like controlled heel slides, single-leg balance work, and resisted side-stepping teach your body how to stabilize without stiffness. These movements activate your deep stabilizers and reinforce good alignment. Importantly, you’ll learn how to carry this stability into your everyday actions so your recovery becomes part of your daily life, not just something you do at the clinic.
Carrying Good Movement into Daily Life
Physiotherapy doesn’t stop when your session ends. In fact, the real progress happens in how you live between visits. You’ll learn how to sit evenly on both hips, stand tall without leaning to one side, and pick things up from the floor without twisting or collapsing into your lower back. You might find yourself shifting your posture during a phone call, gently engaging your glutes as you walk up stairs, or rolling out of bed more mindfully. These micro-adjustments seem small, but over time, they make a big impact. They help you maintain your alignment, avoid flare-ups, and move through your day with less effort and more confidence.
Sustaining Alignment in the Long Term
As your body re-learns how to move well, you start to feel more in control again. You’ll notice that your pain fades, your posture improves, and your balance returns. For some people, occasional physiotherapy tune-ups keep everything in check. For others, a consistent home routine maintains progress. Either way, you gain more than just pain relief, you build body awareness. You move through life more connected to your posture, your breath, and your movement patterns. Whether you’re running, lifting, working, or simply walking your dog, you know how to protect and support your SI joint.
Your Sacroiliac joints may not demand much motion, but they demand your attention when they fall out of sync. With the help of skilled physiotherapy, you can restore balance to your pelvis, calm the chaos of chronic pain, and reclaim the freedom to move with ease. You don’t have to keep pushing through discomfort. Your body knows how to realign. It just needs the right support, the right strategies, and a little time to relearn how to move well.