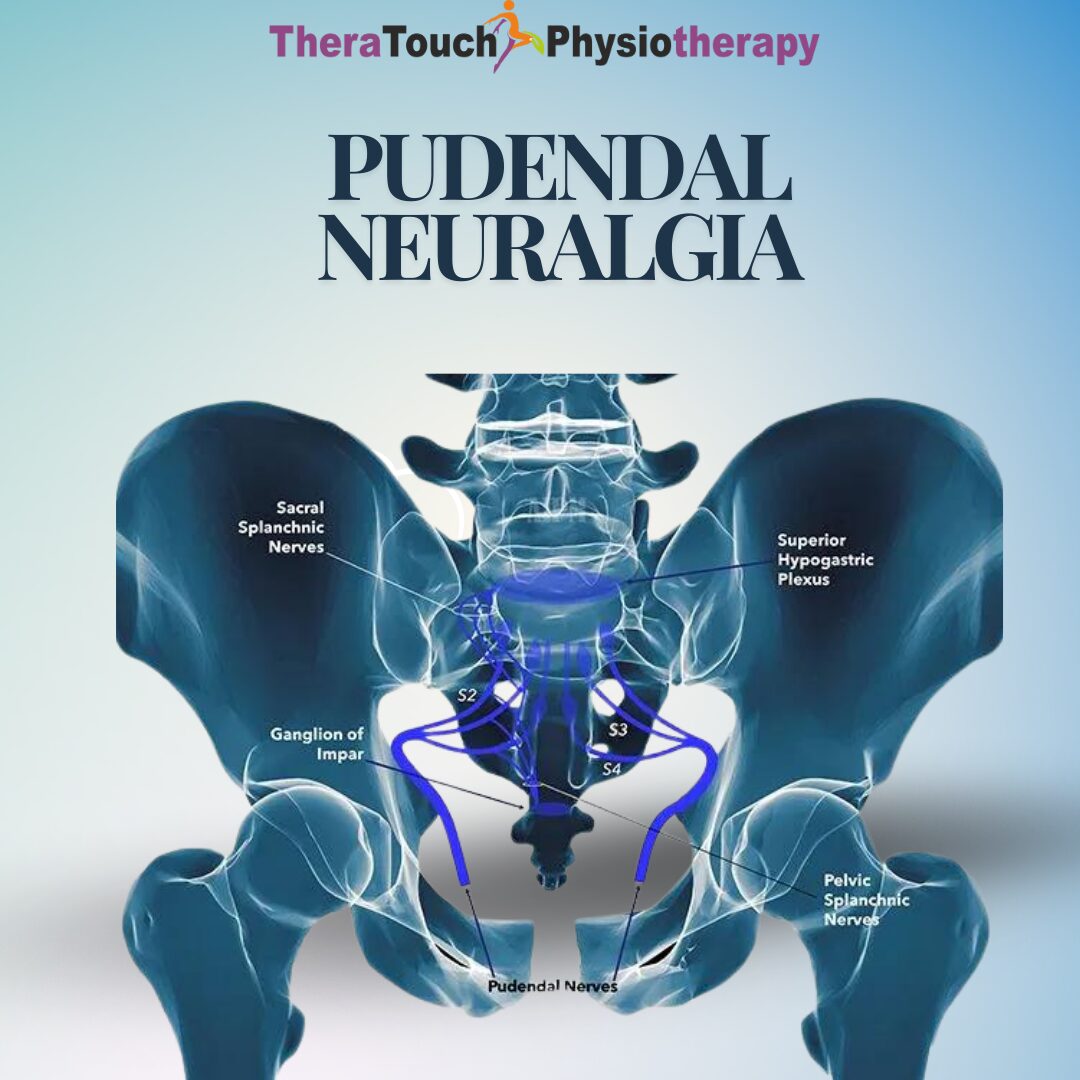
What Pudendal Neuralgia Means for You
Pudendal neuralgia is a chronic pain condition that affects your pudendal nerve, a key nerve in your pelvis that supplies sensation to your pelvic floor, bladder, bowel, and sexual organs. When this nerve becomes irritated, compressed, or damaged, you develop pelvic pain that feels relentless. Because the pudendal nerve controls such intimate areas, the pain can disrupt nearly every aspect of your life from sitting and working to enjoying intimacy or using the bathroom without discomfort.
Many people describe pudendal neuralgia as one of the most life-altering chronic pain conditions. You may feel as if you are sitting on a sharp object or experiencing electric shocks in your pelvic area. The pain often worsens with sitting and improves when you stand or lie down, which makes everyday tasks like commuting, desk work, or social gatherings extremely difficult.
Symptoms You May Experience
The hallmark symptom of pudendal neuralgia is pelvic pain. The pain often feels burning, stabbing, tingling, or electric in nature. It usually affects the areas supplied by the pudendal nerve: the vagina or penis, anus, rectum, perineum, or buttocks.
You may notice that your pain worsens when you sit, especially on firm surfaces, and eases when you stand, lie down, or sit on a specially designed cushion. The discomfort can flare during sexual activity, when you urinate, or when you have a bowel movement. For some people, the pain is constant, while for others it comes in waves or intensifies with certain activities.
Other symptoms may include a feeling of fullness in your rectum or genitals, numbness or tingling in your pelvic region, or hypersensitivity to touch. The emotional toll is also significant. Living with persistent pelvic pain often leads to frustration, anxiety, depression, or a loss of intimacy, making the condition as emotionally draining as it is physically painful.
Causes and Risk Factors
Pudendal neuralgia develops when your pudendal nerve experiences prolonged compression, irritation, or injury. This can occur in several ways. Long hours of cycling, horseback riding, or sitting on hard surfaces can press directly on the nerve and its surrounding tissues. Childbirth can stretch or injure the nerve, especially during long or difficult deliveries. Pelvic surgeries, such as hysterectomy or prostate surgery, sometimes cause scarring that entraps the nerve.
Scar tissue, pelvic floor muscle tension, or anatomical variations in your pelvis can also trap the nerve in narrow spaces. Risk factors include obesity, chronic constipation, repetitive strain, and a history of pelvic trauma. In many cases, no single cause appears, which makes diagnosis more complex.
How Doctors Diagnose Pudendal Neuralgia
Because pudendal neuralgia mimics other pelvic pain conditions such as endometriosis, interstitial cystitis, or chronic prostatitis, diagnosis often takes time. Your doctor will begin by listening to your symptoms in detail. They may perform a physical exam of your pelvis to check for tenderness or nerve sensitivity.
Imaging studies such as MRI may help rule out other causes, but they rarely show pudendal nerve irritation directly. A diagnostic pudendal nerve block is one of the most reliable tests. If your pain improves significantly after your doctor injects anesthetic around the pudendal nerve, it confirms the diagnosis.
The diagnostic process can feel frustrating, but persistence matters. The sooner you receive an accurate diagnosis, the sooner you can start treatment tailored to your needs.
Treatment Options for Pudendal Neuralgia
Treatment usually combines medical, physical, and lifestyle approaches. Your doctor may prescribe medications that target nerve pain, such as gabapentin, pregabalin, or tricyclic antidepressants. These drugs calm overactive pain signals from your nerve. Anti-inflammatory medications or topical numbing creams may help relieve discomfort in localized areas.
Nerve blocks provide another layer of relief. Your doctor injects medication directly around your pudendal nerve, reducing inflammation and calming the pain. These blocks can provide temporary relief and help you tolerate physiotherapy and rehabilitation exercises.
For persistent or severe cases, surgery may be considered. Pudendal nerve decompression surgery involves releasing the nerve from surrounding tissue that compresses it. While not appropriate for every patient, surgery can offer relief for those who do not respond to other treatments.
How Pelvic Floor Physiotherapy Helps You
Pelvic floor physiotherapy plays a critical role in managing pudendal neuralgia. When you live with chronic pain, your pelvic floor muscles often tighten unconsciously in response. This protective guarding makes your pain worse, creating a vicious cycle of nerve compression and muscle tension.
A pelvic floor physiotherapist will assess how your muscles respond to movement and relaxation. They may use gentle internal or external manual therapy to release tight muscles and fascia that place pressure on your pudendal nerve. They will also teach you breathing techniques, posture correction, and exercises that restore healthy coordination between your core and pelvic floor.
Some therapists use biofeedback, which allows you to see how your muscles contract and relax in real time. By retraining your muscles and nervous system, physiotherapy reduces nerve irritation, improves circulation, and restores pelvic function. While physiotherapy does not cure the nerve injury itself, it helps break the cycle of pain and gives you back control over your body.
Daily Strategies You Can Use
Managing pudendal neuralgia requires daily strategies alongside medical care. Using cushions designed for pudendal pain relieves pressure when you sit. Taking regular breaks from sitting, adjusting your posture, and using standing desks help minimize nerve compression. Practicing relaxation techniques such as yoga, meditation, or guided breathing calms your nervous system and lowers pain perception.
Pay attention to diet and hydration. Chronic constipation can aggravate pelvic pain, so a high-fiber diet and plenty of fluids can reduce strain on your pelvic floor. Maintaining a healthy weight decreases unnecessary pressure on your pelvis.
Complications and Long-Term Outlook
If untreated, pudendal neuralgia can become disabling. Persistent pain may lead to loss of mobility, sexual dysfunction, and mental health challenges. However, with early intervention and a comprehensive treatment plan, you can improve significantly. Many people reduce their pain and regain their independence by combining medication, physiotherapy, lifestyle changes, and, when needed, nerve blocks or surgery.
The condition rarely resolves completely on its own, but you can manage it successfully. By building a team that includes your doctor, physiotherapist, and mental health provider, you create a plan that addresses every part of your life affected by pain.
When You Should See a Doctor
You should see a doctor if you have chronic pelvic pain that worsens when you sit and does not improve with basic measures. If pain interferes with your work, intimacy, or daily activities, or if you experience new symptoms such as numbness, bladder problems, or bowel changes, you should seek immediate medical advice. Early diagnosis and treatment make a significant difference in your recovery.
Frequently Asked Questions About Pudendal Neuralgia
What does pudendal neuralgia feel like?
Pudendal neuralgia often feels like burning, stabbing, or electric pain in your pelvic region. The pain usually worsens when you sit and eases when you stand or lie down.
Can pudendal neuralgia go away on its own?
In some cases, symptoms may improve with rest and lifestyle changes, but most people require treatment such as physiotherapy, nerve blocks, or medication.
How long does pudendal neuralgia last?
The condition can last months or years without treatment. With proper care, many people experience significant improvement and return to normal activities.
Does pudendal neuralgia affect sex?
Yes. Pain during or after sex is common because the pudendal nerve supplies sensation to your genitals. Physiotherapy and medical treatment can help improve sexual function.
Can exercise help pudendal neuralgia?
Yes, but you should focus on gentle, nerve-friendly activities such as walking, swimming, or yoga. Avoid cycling or high-impact sports that increase pressure on your pelvis.