C-Section Awareness Month: Road to Recovery
April is C-section Awareness Month, and it’s the perfect time to talk openly about a birth experience that often gets sidelined. A Cesarean section is not just a different way to deliver a baby. It is major surgery. It affects your core, your pelvic floor, your posture, your energy, and your emotions. And yet, many women are sent home with nothing more than basic instructions and told to “take it easy.”
But what happens when the numbness around the scar lingers? When your core feels weak, your bladder feels unreliable, and you can’t quite recognize how your body moves anymore? That’s where real recovery needs to begin. And pelvic floor physiotherapy can play a vital role in supporting you every step of the way.
Understanding the C-Section Experience
A C-section may be scheduled, urgent, or completely unexpected. It can come with relief or disappointment, joy or grief. Sometimes all at once. No matter how it unfolds, it involves incisions through the abdominal wall and uterus, which creates significant changes to your muscles, fascia, and nerves.
Healing from that level of disruption takes more than time. Without guided support, many women struggle with issues like:
- Tight, tender, or numb scar tissue
- Deep core weakness
- Back or pelvic pain
- Bladder leakage or urgency
- Discomfort during sex
- A general feeling of disconnection in the body
These symptoms are common, but they are not something you have to live with.
Why Pelvic Floor Physiotherapy Matters
There’s a common misconception that pelvic floor physiotherapy is only for vaginal births. That couldn’t be further from the truth. Every pregnant person carries their baby with the help of their pelvic floor. During pregnancy, this group of muscles experiences pressure, strain, and postural shifts regardless of the mode of delivery. The pelvic floor also works closely with your core muscles, which are directly affected during a C-section. A pelvic floor physiotherapist understands how these systems work together and how to help you heal safely and fully. We support your journey through every phase; before, during, and after birth.
Before Your C-Section
Pelvic floor therapy before delivery helps prepare your body by improving breathing patterns, posture, and pelvic alignment. It reduces excess tension and teaches you how to engage your deep core muscles properly. These skills can improve surgical outcomes and help you feel more in control going into delivery.
During Hospital Stay and Early Healing
In the early days after a C-section, we introduce gentle movements and breathing techniques to improve circulation, reduce swelling, and ease discomfort. We help you move in ways that support healing and prevent strain, even while getting in and out of bed or caring for your newborn.
After the Initial Recovery Phase
Once your incision heals and you’re cleared to begin movement therapy, pelvic floor physiotherapy becomes even more impactful. We address scar tissue tightness, support safe reactivation of your core, and guide you through progressive strength training that suits your pace and lifestyle. You’ll learn how to lift, move, and return to activity without fear of injury or setbacks. We also treat ongoing symptoms like bladder leakage, heaviness in the pelvis, or pain with intimacy, things that many mothers silently deal with, not knowing help is available.
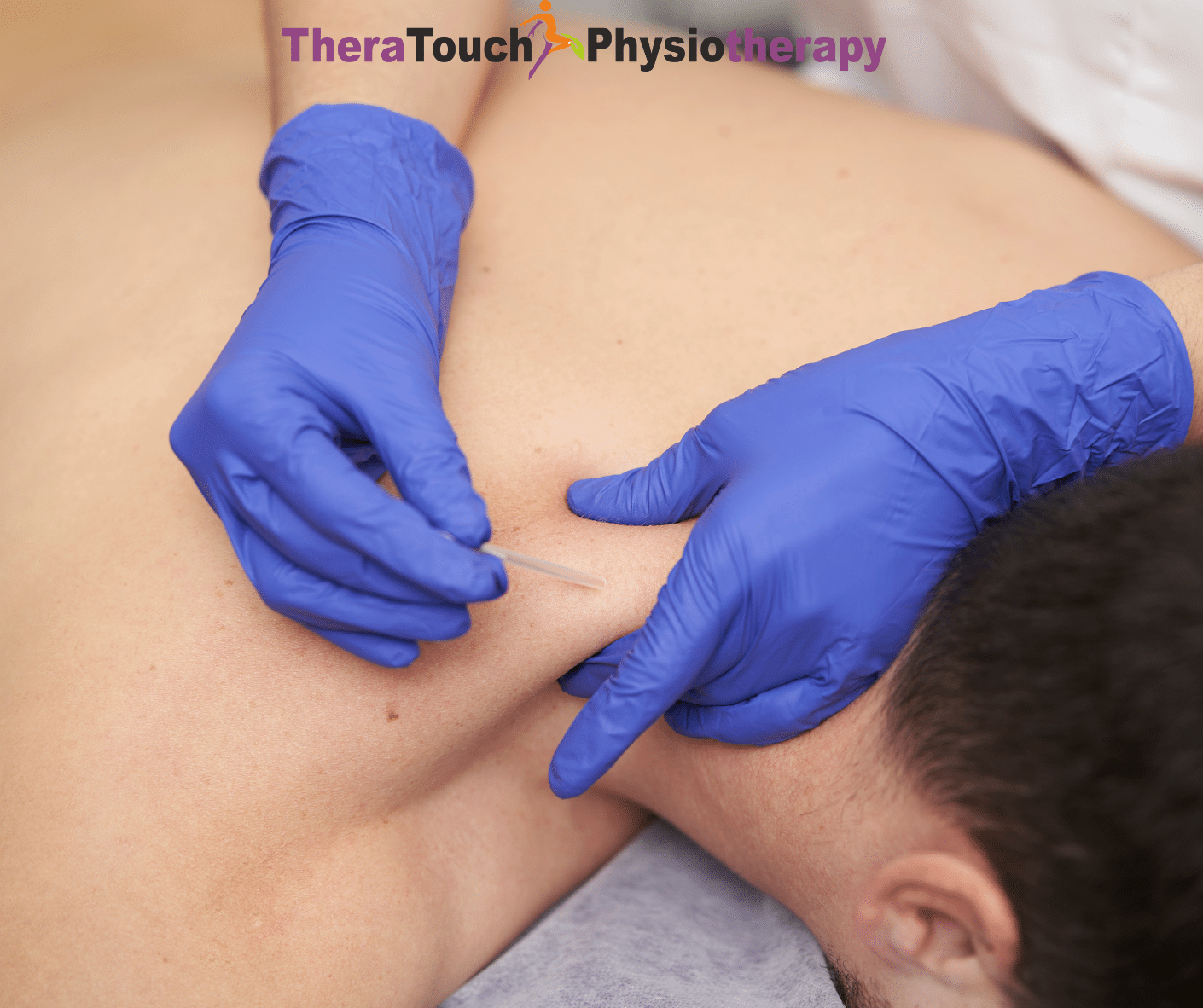
Complementary Services That Support Recovery
At TheraTouch Physiotherapy, we offer more than just pelvic floor therapy. We integrate treatments like dry needling and focused shockwave therapy, which can reduce scar tissue restriction and support soft tissue healing. These treatments improve blood flow, reduce pain, and promote long-term recovery in a non-invasive way. Every session is tailored to your story and your body. There is no one-size-fits-all approach, because no two births or recoveries are the same.
Your Recovery Deserves More Than “Just Rest”
Six weeks is not a magic number. Healing after a C-section is not a countdown. It is a journey of reconnecting with your body, regaining strength, and building confidence in how you move, parent, and live. Including a pelvic floor physiotherapist on your postpartum care team can make a real difference in how you feel now and, in the years, ahead. Whether it has been weeks or years since your C-section, you are not too late to begin.
Let’s Change the Conversation Around C-Section Recovery
C-section Awareness Month is about more than statistics and scar stories. It is about acknowledging the courage, complexity, and strength it takes to recover from a surgical birth. It is about making sure no mother feels forgotten in her healing process. At TheraTouch Physiotherapy, we are proud to walk alongside you. We offer the care, tools, and guidance that help you restore, rebuild, and truly recover. If you are ready to begin or continue your healing journey, we are here. Let’s take the next step together.