Plantar Fasciitis: Understanding Heel Pain
Plantar fasciitis causes millions of people to start their day with pain. That first step out of bed feels like stepping on a knife. A sharp, stabbing sensation near the heel. The discomfort eases a little with movement, only to return after sitting too long or walking too far. For many, this cycle continues for months, sometimes years, without relief.
This condition, though common, often frustrates patients because rest, ice, and over-the-counter painkillers don’t offer long-term solutions. However, when you understand how plantar fasciitis works and how physiotherapy treats its root causes, you gain the knowledge to recover, prevent flare-ups, and reclaim pain-free movement.
What Happens to the Plantar Fascia
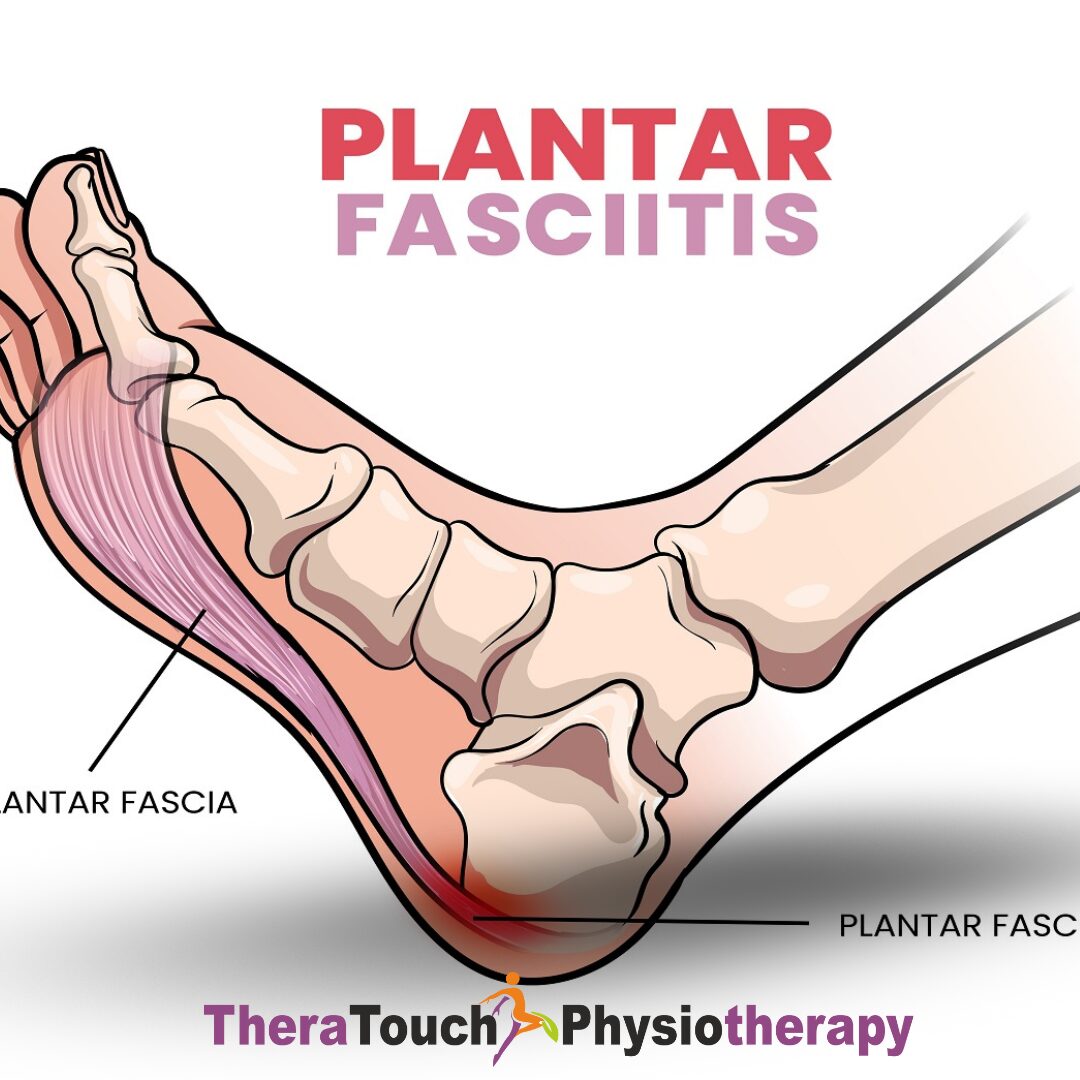
Your plantar fascia is a thick band of connective tissue that stretches along the bottom of your foot, from your heel bone to your toes. It supports your arch and helps your foot absorb shock with every step. When you walk, run, or stand, the fascia absorbs force and stores energy like a spring, then releases it as you push off the ground.
If you overload this structure by running too much, standing too long, wearing unsupportive shoes, or having poor foot mechanics, the fascia starts to strain and develop tiny tears. Instead of healing properly, it reacts with irritation and stiffness. Over time, it becomes less flexible, more inflamed, and painfully sensitive.
You feel the worst pain when you first put weight on the foot after a period of rest. That’s because the fascia tightens overnight, and when you step down in the morning, the sudden stretch reopens those microtears.
How Plantar Fasciitis Changes Daily Life
Plantar fasciitis does more than affect your foot. It disrupts your routine. You start avoiding walks. You sit more. You compensate by shifting weight onto your other foot or limping. These small adjustments change how your entire body moves.
If you ignore the pain, your gait can change so much that your knees, hips, or lower back begin to hurt. Your body adapts to protect the injured foot, but in doing so, it creates new problems.
People often believe the pain will disappear with time. But for many, it doesn’t. It stays, worsens, or flares up again months later. That’s because they treat the pain, but not the dysfunction causing it.
Why This Condition Develops
Plantar fasciitis develops slowly in most people. It doesn’t begin with one injury. Instead, repetitive stress builds over time.
Runners may add mileage too quickly. Office workers might walk in flat shoes without arch support. Healthcare and hospitality workers often spend long hours on hard floors. In all these cases, the foot takes more load than it can manage, and the fascia breaks down.
Biomechanics also play a role. People with flat feet or high arches shift load through the foot abnormally. Tight calf muscles and stiff ankles reduce the foot’s ability to move well. Extra body weight increases the load on the fascia during every step. Even standing still if done repeatedly and without support can cause damage.
How Physiotherapists Diagnose the Condition
A physiotherapist identifies plantar fasciitis based on your history and symptoms. They ask when the pain began, when it feels worse, and how it limits your activity. Then, they examine your foot and test where the pain occurs.
They check the tightness of your calves, the range of your ankle, the strength of your foot muscles, and the way you walk. Sometimes, they analyze your gait on video to catch movement errors that contribute to the problem.
You don’t usually need an X-ray or MRI to diagnose plantar fasciitis. But if your pain doesn’t follow typical patterns or fails to improve with care, imaging can help rule out fractures, nerve irritation, or other heel conditions.
Why Physiotherapy Works
Physiotherapy works because it addresses both the symptoms and the reasons why the fascia broke down. Instead of treating only the pain, your physiotherapist rebuilds your movement from the ground up.
At first, they may use hands-on techniques to reduce tissue tension and pain. These include massage, myofascial release, or joint mobilization. They might tape your foot to support the arch and reduce stress on the fascia.
As you improve, they introduce stretches that target your calf muscles, Achilles tendon, and plantar fascia. These restore mobility to the ankle and foot. Strengthening exercises come next. Your therapist teaches you how to activate the small muscles inside your foot and the larger muscles in your hips and legs that support good walking mechanics.
In later stages, they help you retrain your gait. They show you how to land more evenly, push off with better control, and absorb force without overloading the heel. If needed, they recommend footwear, orthotics, or shockwave therapy. Throughout the process, they educate you so you understand how to manage the condition and prevent its return.
A Real-Life Recovery
Angela, a 44-year-old teacher, spent most of her workdays on her feet. After months of growing heel pain, she started limping in the mornings and sitting between classes. She tried home stretches and bought expensive insoles, but nothing worked.
When she started physiotherapy, her therapist found that she had very tight calves, poor ankle mobility, and weak gluteal muscles. Her therapist treated the fascia manually and gave her a daily stretching program. Over the next six weeks, Angela progressed to foot-strengthening drills and gait retraining.
By week ten, Angela was walking without pain. She had returned to teaching full-time without needing breaks. Just as importantly, she understood why the pain developed and how to keep it from coming back.
What to Expect From Recovery
Recovery from plantar fasciitis takes time, but most people improve within six to twelve weeks with consistent physiotherapy. Severe or long-standing cases may take longer, especially if the fascia has undergone significant degeneration.
Rest alone won’t fix the problem. If you stop moving altogether, the fascia becomes stiffer and weaker. But if you overload it without guidance, you may flare up the pain. That’s why working with a physiotherapist is so important. They adjust your plan to match your stage of healing.
They also help you set expectations. Healing the fascia involves rebuilding load tolerance and correcting biomechanics not just waiting for the pain to fade. But once you address the root cause, your chances of long-term success are high.
Don’t Wait to Take the First Step
Plantar fasciitis does more than cause heel pain. It changes how you move, limits your independence, and affects your confidence. But with physiotherapy, you can break the cycle. You don’t have to live with fear of the first step in the morning. You don’t have to stop doing what you love. You just need the right plan, the right guidance, and the commitment to move forward. Physiotherapy doesn’t just treat plantar fasciitis. It helps you take back your stride, one strong, supported step at a time.