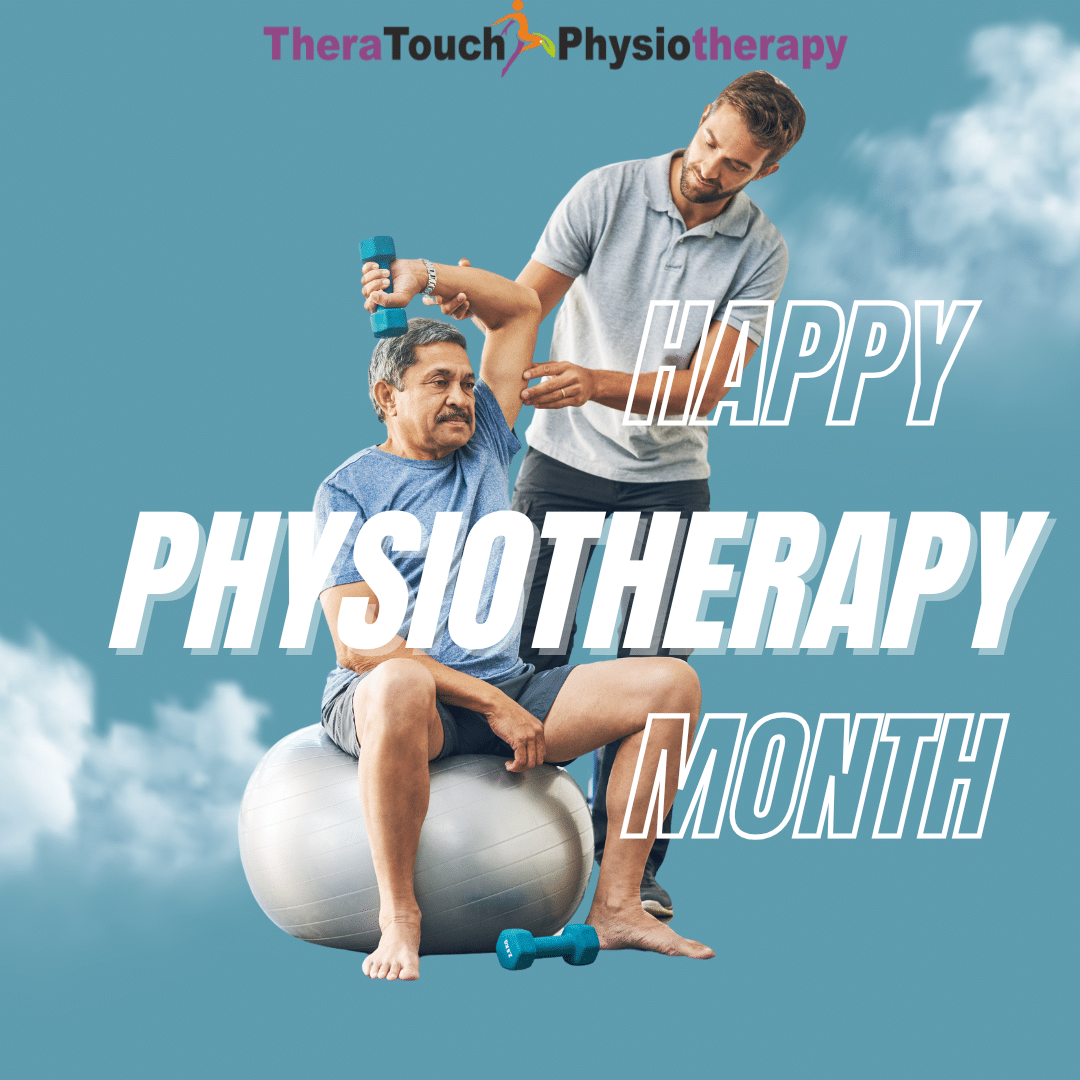
Physiotherapy Month: Why Your Health Deserves the Spotlight
May arrives with more sunlight, longer days, and a natural invitation to move more and feel better. At TheraTouch, May also carries a deeper meaning. It is Physiotherapy Month, and we are taking this time to celebrate the power of movement, healing, and health awareness.
Physiotherapy is often misunderstood. Some people think it is just exercise. Others believe it is only for injuries. But physiotherapy is one of the most effective and empowering ways to improve your health. It supports your physical, mental, and emotional well-being
What Is Physiotherapy Month About?
Physiotherapy Month is a chance to celebrate everything that physiotherapy brings into our lives. It brings pain relief, yes, but it also brings freedom, helps people recover and rebuild and strengthens not just bodies, but confidence.
This month, we are starting conversations. We are sharing stories. Most importantly, we are reminding you that your body deserves attention before pain forces you to stop.
Let’s Talk About Health Awareness
May also brings a spotlight on health issues that often go unnoticed or undiscussed. At TheraTouch, we believe that understanding your health is the first step to protecting it.
Pelvic Health Is Important
Incontinence, and postpartum discomfort are common, but often kept quiet. We offer relief, strength, and control. You do not have to suffer in silence. We are here to help you reconnect with your body and feel more confident in it.
Injury Prevention Matters
You do not have to wait for an injury to see a physiotherapist. We help you prevent problems before they start. Whether you play sports, love the gym, or simply want to move better in your everyday life, we assess your movement patterns and help you build long-term strength and flexibility.
Posture, Breathing, and Chronic Pain Are Connected
Poor posture and shallow breathing are common in today’s fast-paced world. These habits often lead to tension and chronic pain. With the right support, you can learn better ways to move, stand, sit, and breathe. These small changes can lead to big results.
Mental Health Starts with Physical Care
Stress lives in the body. You can feel it in your neck, shoulders, and back. When you take care of your body, your mind begins to feel lighter too. Physiotherapy creates space for your body to relax and heal, and that can make a real difference in your emotional well-being.
A Personal Invitation
If you have been living with discomfort, if you have been waiting for the right moment, let this be it. Your body is speaking. We are here to listen.
This May, do something kind for yourself. Book a session. Learn something new about your health. Talk to a physiotherapist. Encourage a loved one to do the same.
Physiotherapy is not just about getting you back to where you were. It is about helping you become your strongest, most confident self.
This month be a fresh start.
Let it be the beginning of a better relationship with your body.
It should remind you that healing is possible, and that you deserve it.
We are here for you.
Contact TheraTouch Physiotherapy to begin your journey.
We can’t wait to walk with you toward better health.