What Lower Back Pain Indicates
Your lower back pain does not arrive without warning or cause. Even if the discomfort seems sudden, your body has likely been giving you clues for a while. You might feel a sharp pull after bending or lifting something heavy, or perhaps a dull persistent ache creeps in after hours of sitting. These sensations are not isolated, they are signals that your body is working hard to compensate for weaknesses, imbalances, and faulty movement habits that have built up over time.
Lower back pain often reflects a mismatch between the demands placed on your body and the support your core and spinal structures provide. When muscles around your spine do not activate properly or when you rely too heavily on one side of your body, your lower back becomes the default stabilizer. The more it overworks, the more vulnerable it becomes to strain and inflammation. Your pain becomes a message your spine and supporting muscles are struggling to meet your daily demands, and they need your attention.
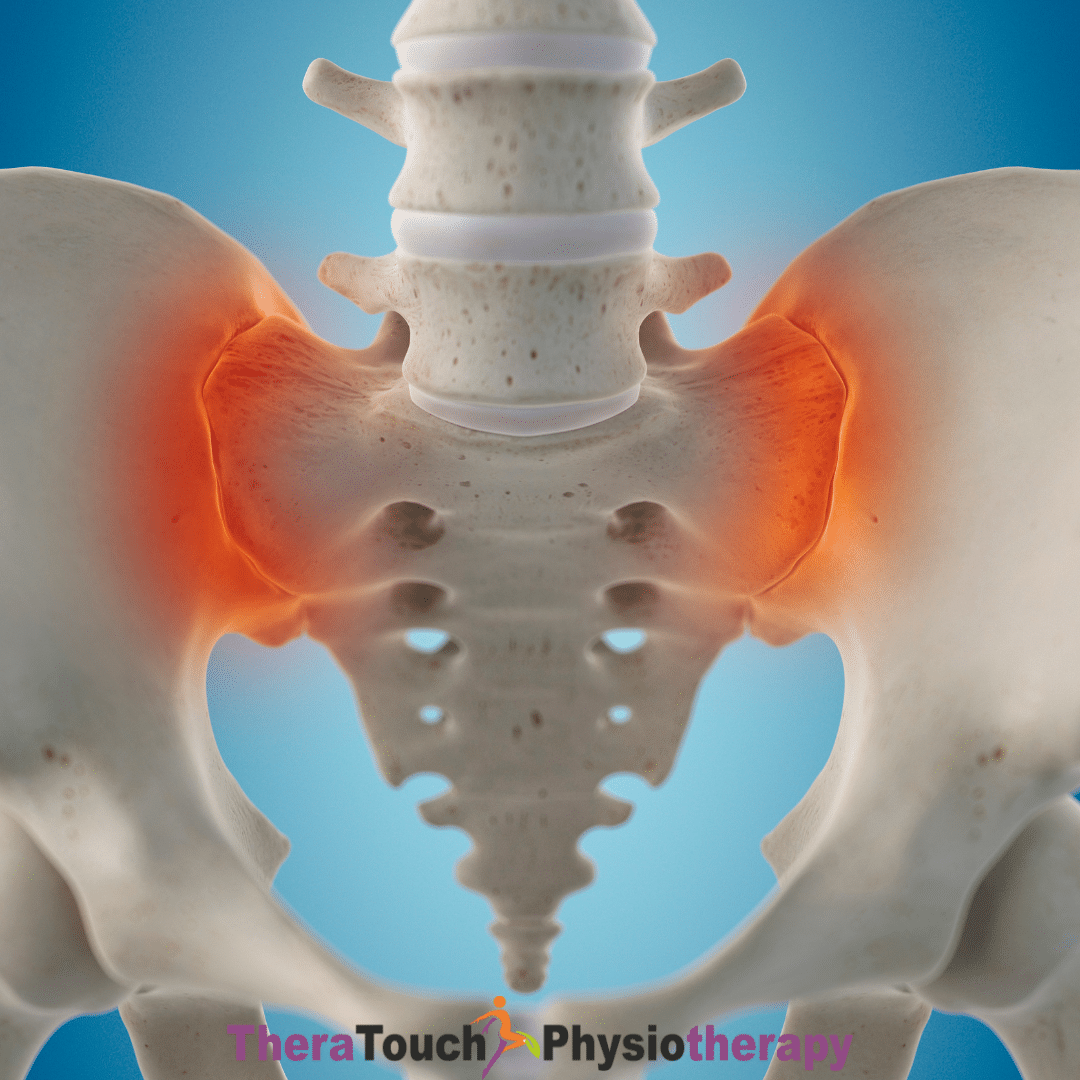
You may also experience back pain because of tight hip flexors pulling your pelvis forward, weak glutes that no longer support your movements, or a stiff upper back that forces your lower back to overcompensate. It could even be that your breathing patterns and posture increase spinal pressure over time. All of these factors contribute to the imbalance and overload that eventually show up as pain.
How Rest Alone Falls Short
When pain strikes, you might instinctively stop all movement. You may lie down, reduce your activity, or avoid certain motions that provoke discomfort. While this initial rest can help calm inflammation, it does not address the reasons the pain developed in the first place. In fact, prolonged inactivity can do more harm than good.
Resting completely slows your blood flow, reduces the natural lubrication of your joints, and causes your muscles to weaken. As your muscles lose tone and coordination, your spine becomes even less supported. Once you return to your usual activities, you may find that your pain returns sometimes more intense and persistent than before.
Instead of only avoiding movement, you need to retrain how your body moves. Movement done mindfully and with proper guidance helps restore your body’s balance and function. That’s where physiotherapy plays a critical role.
How Physiotherapy Offers Active Solutions
At TheraTouch, your physiotherapist takes a thorough approach to understanding the root cause of your lower back pain. They begin by learning how you move, how you breathe, how you distribute your weight when you walk or stand, and how you perform simple tasks like bending, lifting, or reaching. They examine the quality of your spinal mobility, the strength of your core muscles, and your joint alignment.
By evaluating your posture and identifying movement restrictions or compensations, your therapist pieces together a complete picture of what is stressing your lower back. Once the problem areas are clear, they use gentle manual techniques to release stiff joints and tight muscles. They also begin teaching you how to move in ways that protect and support your spine.
Physiotherapy does not just treat your pain. It helps you relearn how to move, breathe, and support your body so that you reduce the likelihood of the pain returning.
How You Rebuild Spinal Stability
A major part of your recovery involves restoring the deep core muscles that stabilize your spine from within. These muscles, such as the transverse abdominis and multifidus, work in harmony with your breathing and posture. But when they are weak or uncoordinated, your body recruits other muscles to compensate, which adds more strain to your lower back.
Your physiotherapist teaches you how to engage these muscles in small, subtle ways that do not involve bracing or holding your breath. You learn to create internal stability through gentle but consistent control. These exercises progress slowly and intentionally. You start with basic breath-linked movements and build up to more functional tasks like rolling, getting in and out of bed, or carrying items safely.
The goal is not just to strengthen but to create balance. You want your muscles to respond when needed and relax when appropriate. You rebuild spinal stability by restoring muscle timing and reducing the reliance on compensatory patterns.
How You Reinforce New Movement Patterns to avoid Lower back Pain
Once you regain stability, you need to apply that control to everyday life. Your therapist works with you to relearn common actions in a way that protects your back. You learn how to lift without using your lower back as the primary mover. You discover how to transition from sitting to standing smoothly and how to move from side to side without twisting or wrenching your spine.
These lessons become part of your daily routine. They help you move with confidence instead of fear. By practicing these patterns consistently, you prevent your old habits from creeping back in. You begin to live with movement that feels safe, strong, and efficient.
How You Reduce Recurrence of Lower Back Pain
As your new habits take hold, you begin to experience tangible relief. Your back feels less stiff when you wake up. You move more freely throughout the day. Your core feels stronger and more connected. Tasks that once triggered pain feel manageable again.
This progress not only improves your comfort but also reduces the chance of future pain episodes. Your joints stay mobile. Your muscles support you in harmony. You stop relying on temporary fixes like painkillers or hot packs. You begin to trust your body again and feel capable of handling movement and activity without worrying about injury.
How TheraTouch Supports Your Journey
At TheraTouch Physiotherapy, you receive more than exercises and massage. You receive a personalized treatment plan designed around your unique needs, lifestyle, and goals. Your therapist walks with you every step of the way, adjusting your program as your body heals and adapts. They make sure your progress continues without plateauing.
TheraTouch combines hands-on manual therapy, functional movement retraining, breathing integration, and posture education to help you build a resilient spine. Your sessions focus not just on what hurts but on what caused it, how to prevent it, and how to keep your body moving well into the future.
Your lower back pain is not something you need to live with or ignore. It is a sign that your body is calling out for support, stability, and balanced movement. When you understand what your pain is telling you and take the right steps to address it, you give your body the chance to heal in a lasting way.
With the right care, you can move freely again, stand and sit with comfort, and return to the activities you love without fear. TheraTouch is here to guide you through every phase of that recovery, offering the tools, knowledge, and encouragement you need to build strength from the inside out.